- What is MIPS?
- What are the differences between MIPS 2023 and MIPS 2024?
- Who has to report MIPS?
- Can providers participate in MIPS as an individual provider or a group practice?
- What are the MIPS Categories?
- What determines my final MIPS Score (CPS)?
- What happens if I report less than 6 measures?
- What impact does MIPS have on my Medicare payments and clinical reputation?
- What is the minimum amount of MIPS data I have to report to avoid a penalty in?
- Is there flexibility within MIPS for Small Practices?
- How do I get started reporting MIPS through MDinteractive?
- What are MIPS Value Pathways (MVPs)?
What is MIPS?
The Merit based Incentive Payment System (MIPS), established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), came into effect on January 1, 2017. It is a major catalyst towards transforming the healthcare industry from fee-for-service to pay-for-value.
MIPS rolled 3 existing quality and value reporting programs (PQRS, VBM and MU) into one points based program.
MIPS annually scores eligible Medicare Part B clinicians on a 100-point performance scale which results in a Composite Performance Score (CPS). The payment adjustment will be based on this Composite Performance Score which is calculated by the measures and categories reported. MIPS is designed to be a budget-neutral program. 2022 was the last performance period with an exceptional performer bonus (based on the number of points achieved).
The Quality Payment Program (QPP) consists of two major tracks:
- The Merit-based Incentive Payment System (MIPS)
- Alternative Payment Models (APMs)
Most providers will initially participate through MIPS.
The 4 MIPS categories are:
- Quality (30% of score)
- Promoting Interoperability (25% of score)
- Improvement Activities (15% of score)
- Cost (30% of score)
What are the differences between MIPS 2023 and MIPS 2024?
| Rules | MIPS 2023 | MIPS 2024 |
|---|---|---|
| Low Volume Threshold to be Eligible |
| No change |
| Determination Periods | Two Determination Periods for the Low-Volume Threshold (LVT):
|
The MIPS determination period includes two 12-month segments:
|
| Payment Adjustment Range | -9% to +9x% | No Change |
| Minimum MIPS score to avoid penalty | 75 points | No Change |
| Exceptional Performance Threshold | Retired | Retired |
| Cost Category Weight | 30% | No Change |
| Bonus Points |
| No Change |
Who has to report MIPS?
- MIPS eligible clinicians who bill for Medicare Part B (otherwise known as the Physician Fee Schedule) or Critical Access Hospital (CAH) Method II payments assigned to the CAH and meet the low volume threshold (LVT) include:
- Physicians (MD/DO, DDS, DDM, DPM, Optometrists, and Chiropractors)
- Osteopathic Practitioners
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Certified registered nurse anesthetists
- Physical or occupational therapists
- Speech-language pathologists
- Qualified audiologists
- Nurse midwives
- Clinical psychologists
- Dieticians/nutritional professionals
- Clinical social workers
- Certified nurse-midwives
- Could I be exempt from MIPS?
- Yes! The following clinicians are exempt from MIPS:
- Newly enrolled in Medicare (exempt until the following performance year)
- Clinicians meeting a low-volume threshold ($90,000 or less in billed Medicare Part B allowed charges for covered professional services, or provide care for 200 or fewer Medicare Part-B enrolled patients, or deliver less than 200 covered services to Part B beneficiaries in one year)
- Clinicians significantly participating in "alternative payment models" (APMs)
- Note: MIPS non-eligible clinicians may be able to "opt-in" to report (and be subject to a MIPS payment adjustment) or could "voluntarily" report (but will not be subject to the MIPS payment adjustment)
- To check if you need to submit MIPS data, please visit the CMS MIPS Participation Status website.
- Yes! The following clinicians are exempt from MIPS:
- What is the MIPS Extreme and Uncontrollable Circumstance Policy?
- Extreme and uncontrollable circumstances are defined as rare events entirely outside of your control and the control of the facility in which you practice.
- Clinicians impacted by natural disasters (as an example) can claim the hardship exception for all the performance categories - Quality, Cost, Improvement Activities, and Promoting Interoperability.
- The deadline for the hardship exception application is December 31.
- CMS Exception Applications
Can clinicians participate in MIPS as an individual clinician or a group practice?
- Clinicians can choose to participate in MIPS as either:
- An Individual (defined as a single National Provider Identifier (NPI) tied to a single Tax Identification Number (TIN); OR
- A group (defined as at least 2 clinicians (identified by their individual NPIs) sharing a common TIN). At least 1 clinician must be individually eligible for MIPS.
- Important: The decision to report individually or as a group, applies across all MIPS categories for a given performance year. A clinician cannot choose to report as an individual in some categories while reporting as a group for other categories. The decision to report as a group or by individual clinicians has financial and reputational ramifications that should be taken into consideration.
- Individual Reporting:
- The data is reported for every eligible clinician in the group for all four MIPS performance categories (or for just the categories the clinician chooses to submit).
- The MIPS score will be calculated based on the individual performance reported, and the payment adjustment will be calculated accordingly.
- Clinicians billing CMS with two (or more) different TINs would possibly need to report each combination and would, in this scenario, receive MIPS scores and separate payment adjustments for each TIN/NPI combination. The QPP participation tool will provide information on the clnician's practices.
- Group Reporting:
- A group will be measured as a group practice across all 4 MIPS performance categories (or just the categories they choose to report/attest to). Data is aggregated at the group-level for each of the MIPS categories and then reported.
- All the eligible clinicians in the group will get one MIPS score based on the group’s performance.
- There is no CMS enrollment process or deadline for reporting as a group.
- An organization must include the data from all the clinicians in the group, including clinicians who are otherwise excluded from MIPS individually due to low volume, newly Medicare enrolled status, or QP status from an Advanced APM.
- Individual Promoting Interoperability data can be excluded from group reporting for some clinician types such as non-patient facing or hospital-based clinicians. Their data must be included in the other categories for group reporting but the group can choose to remove them from the TIN level data for PI.
- Virtual Group Reporting:
- Virtual Groups are composed of solo practitioners and groups of 10 or fewer eligible clinicians, eligible to participate in MIPS, who come together “virtually” with at least 1 other such solo practitioner or group to participate in MIPS for a performance period of a year. A virtual group is a combination of 2 or more Taxpayer Identification Numbers (TINs) that elect to form a virtual group for the performance year. There isn't a limit to the number of TINs composing a virtual group.
- A solo practitioner or group can only participate in 1 virtual group in any performance period. But, there are no limits on how many solo practitioners and groups can join a virtual group.
- If a group chooses to join a virtual group, all of the eligible clinicians in that group have to be included in the virtual group. Any group that wants to be part of a virtual group must have 10 or fewer eligible clinicians.
- The majority of MIPS group scoring rules apply to virtual groups.
- Clinicians in a Virtual Group will report as a Virtual Group across all 4 performance categories (or just the categories they choose to report) and will need to meet the same measure and performance category requirements as non-virtual MIPS groups.
- Solo practitioners and groups who want to form a virtual group must go through an election process. Virtual groups election must occur prior to the beginning of the performance period and cannot be changed once the performance period starts. The election period was October 3 to December 31, 2023, for the 2023 MIPS performance period.
- In order to participate in MIPS as a virtual group for the 2024 performance period, virtual groups are required to have submitted an election to CMS via e-mail (MIPS_VirtualGroups@cms.hhs.gov) by December 31, 2023.
What are the MIPS Categories?
Providers participating in the MIPS program will receive a “composite performance score” based on their performance in 4 categories:
| 30% of total score |
| 25% of total score |
 Improvement Activities | 15% of total score |
| 30% of total score |
More details about MIPS Categories...
Quality Details - 30% of score*
- Report 6 measures with one Outcome, or if no Outcome applicable, another High Priority measure (Appropriate Use, Patient Safety, Efficiency, Patient Experience, or Care Coordination).
- Data Completeness: Each measure is reported on 100% of denominator eligible encounters - entire year, all insurances. Answers (numerator options) must be provided for at least 75% of eligible cases**.
- Measures must have at least 20 records in the denominator (and meet data completeness) to be scored against national benchmarks.
- A clinician may choose to report a specialty measure set, defined by CMS for a particular specialty. If a specialty measure set contains fewer than 6 measures, then a clinician could still achieve the maximum possible score for the Quality category by reporting all the measures in the measure set. Specialty measure sets are identified in the Suggestions by Specialty page which can be found here.
- If a clinician cannot identify 6 applicable measures, they may still be able to achieve the maximum score in the Quality category by passing a validation process called Eligible Measure-Applicability (EMA)
*This weight will be 55% if provider/group is exempt from PI or if Cost cannot be calculated.
**View the list of the 2024 Quality measures with documentation here.
Promoting Interoperability Details - 25% of score - 180 days minimum reporting period
- What is PI? This performance category promotes patient engagement and electronic exchange of information using certified electronic health record technology (CEHRT).
- Objective: e-prescribing
- e-Prescribing (10 points)**
- Query of Prescription Drug Monitoring Program (PDMP) (10 points)
- Objective: Provider to Patient Exchange
- Objective: Health Information Exchange - Option 1 (2 measures) OR Option 2 OR Option 3
- Option 1: Support Electronic Referral Loops by Sending Health Information (15 points)**
- Option 1: Support Electronic Referral Loops by Receiving and Incorporating Health Information (15 points)**
- OR
- Option 2: 1: HIE Bi-Directional Exchange (30 points)
- OR
- Option 3: Enabling Exchange Under TEFCA (30 points)
- TEFCA - Trusted Exchange Framework and Common Agreement.
- The MIPS eligible clinician or group must attest to the following: Participating as a signatory to a Framework Agreement (as that term is defined by the Common Agreement for Nationwide Health Information Interoperability as published in the Federal Register and on ONC’s website) in good standing (that is, not suspended) and enabling secure, bi-directional exchange of information to occur, in production, for every patient encounter, transition or referral, and record stored or maintained in the EHR during the performance period, in accordance with applicable law and policy.
- Using the functions of certified electronic health information technology (CEHRT) to support bi-directional exchange of patient information, in production, under this Framework Agreement. First proposed in January 2018 by ONC, TEFCA aims to increase and enhance interoperability and improve the ability of providers and their patients to securely access and use data from different sources. It includes two parts – a Trusted Exchange Framework and a Common Agreement.
- TEFCA - Trusted Exchange Framework and Common Agreement.
- Objective: Public Health and Clinical Data Exchange (report 2 required measures for 25 points)
- Immunization Registry Reporting - required**
- Electronic Case Reporting- required**
- Bonus points available:
- Syndromic Surveillance Reporting
- Public Health Registry Reporting
- Clinical Data Registry Reporting
- **There are exclusions available for most of the PI measures. If you meet and claim the exclusion for one or more of the required Promoting Interoperability performance category measures, the points for the measure will be redistributed to another measure or measures.
- In addition to submitting measures, clinicians must complete the following attestations:
- Submit a “yes” to the Actions to Limit or Restrict Compatibility or Interoperability of CEHRT (previously named the Prevention of Information Blocking) Attestation,
- The ONC Direct Review Attestation (this is an optional attestation, you may attest “yes” or “no”); and
- Submit a “yes” for the security risk analysis measure.
- Submit a "yes" for the Safety Assurance Factors for EHR Resilience (SAFER) Guides Measure (Updated for 2024: a "no" will no longer satisfy this measure).
- How is PI Category reweighted?:
- Automatic Re-weighting: PI will automatically be re-weighted to 0% (and weight will be added to the quality category - making it 55% of total score) without submitting an application for:
- Hospital-based MIPS eligible clinicians - >75% of the MIPS eligible clinicians in the group being hospital-based
- Non-Patient-Facing clinicians or groups with >75% NPF clinicians
- Ambulatory Surgical Center (ASC) based MIPS eligible clinicians
- Small practices (less than 16 in the TIN as designed by QPP)
- Clinical Social Workers
- If you qualify for automatic re-weighting you can still choose to report if you’d like. In this scenario, PI will become 25% of your score and Quality will not be re-weighted.
- If reporting as a group, all MIPS eligible clinicians in the group must qualify for re-weighting with the exception of non-patient facing category. To be designated as a non-patient facing group, 75% of the clinicians in the group must be non-patient facing.
- Automatic Re-weighting: PI will automatically be re-weighted to 0% (and weight will be added to the quality category - making it 55% of total score) without submitting an application for:
- Re-weighting by Hardship Exception Application: Eligible clinicians can submit an application by December 31 to claim the hardship exception and get the PI category re-weighted to 0% (and weight added to the Quality category). Clinician will qualify to file for an exception in the following situations:
- Clinicians whose EHR was decertified during the performance year
- MIPS Eligible Clinicians facing significant hardship defined as:
- Have insufficient internet connectivity
- Extreme and uncontrollable circumstances (e.g. Natural Disasters, practice closure, financial distress, vendor issues)
- Lack of control over the availability of CEHRT
- Note: Not having CEHRT is not sufficient by itself to qualify for re-weighting.
- CMS Exception Applications
Improvement Activities (IA) Details: - 15% of Score
- What is IA? IA rewards clinicians for delivering care that emphasizes care coordination, beneficiary engagement and patient safety.
- Performance in this category is calculated based on the provider’s attestation to completing 2 high-weighted activities or 4 medium-weighted activities* for a minimum of 90 continuous days during the reporting period.
- *Special scoring consideration is given to:
- small practices (less than 15 in the TIN),
- rural practices,
- health professional shortage areas (HPSAs),
- or non-patient facing clinicians.
- These categories of providers are only required to report 1 high-weighted OR 2 medium-weighted activities for full participation.
- Groups must have at least 50% of the clinicians completing the activity/activities that they have chosen to attest to.
- If 50% of the practice sites within a TIN are certified as Patient Centered Medical Home (PCMH), the TIN will earn full credit for the IA category.
- View the list of Improvement Activities and the Data Validation criteria here .
Cost - 30% of Score
- The Cost performance category reporting period is calculated based on the full year.
- A total of 29 cost measures are used to evaluate performance in the Cost performance category.
- No submissions will be required for the Cost category. The Cost category score will be calculated from Medicare administrative claims.
- Similar to the calculation of Quality performance category score, the Cost score will be calculated by comparing performance against benchmarks and the points will be assigned on a decile system. However, the benchmarks for Cost measures will be based on the same year’s performance, unlike the Quality benchmarks which are based on historical performance.
- A maximum Cost improvement score of one percentage point out of 100 is established for this category.
- Each measure will be scored only if the reporting entity meets the case minimum requirement for the measure. For 2024, the minimum number of cases required for each measure are:
- Medicare Spending Per Beneficiary Clinician (MSPB) – 35 episode minimum
- ITotal Per Capita Cost for all attributed beneficiaries - 20 Medicare Patients minimum
- 27 episode-based measures - Minimum case episodes per type: 10 = procedural measures (except Colon and Rectal resection which has 20 case min); 20= Acute Inpatient, Chronic and Emergency Medicine
- Knee Arthroplasty - Procedural
- Elective Outpatient Percutaneous Coronary Intervention (PCI) - Procedural
- Revascularization for Lower Extremity Chronic Critical Limb Ischemia - Procedural
- Routine Cataract Removal with Intraocular Lens (IOL) Implantation - Procedural
- Screening/Surveillance Colonoscopy - Procedural
- Acute Kidney Injury Requiring New Inpatient Dialysis - Procedural
- Elective Primary Hip Arthroplasty - Procedural
- Femoral or Inguinal Hernia Repair - Procedural
- Lumbar Spine Fusion for Degenerative Disease, 1–3 Levels - Procedural
- Lumpectomy Partial Mastectomy, Simple Mastectomy - Procedural
- Non-Emergent Coronary Artery Bypass Graft (CABG) - Procedural
- Renal or Ureteral Stone Surgical Treatment - Procedural
- Melanoma Resection - Procedural
- Colon and Rectal Resection - Procedural
- Intracranial Hemorrhage or Cerebral Infarction - Acute Inpatient
- ST-Elevation Myocardial Infarction (STEMI) with Percutaneous Coronary Intervention (PCI) - Acute Inpatient
- Hemodialysis Access Creation - Procedural - Acute Inpatient
- Inpatient Chronic Obstructive Pulmonary Disease (COPD) Exacerbation - Acute Inpatient
- Lower Gastrointestinal Hemorrhage (*only for groups) - Acute Inpatient
- Psychoses and Related Conditions - Acute Inpatient
- Sepsis - Acute Inpatient
- Diabetes - Chronic Condition
- Asthma/COPD - Chronic Condition
- Depression - Chronic Condition
- Heart Failure - Chronic Condition
- Low Back Pain - Chronic Condition
- Emergency Medicine - Care Setting
- If only one measure can be scored, the performance on that measure will determine the Cost category score.
- Cost Performance in the MVP Reporting Option Performance is calculated exclusively on the cost measures that are included in the selected MVP using administrative claims data, even if additional cost measures (outside your selected MVP) are available for scoring. You’ll only be scored on measures for which you meet or exceed the established case minimum.
- If none of the measures can be scored, the MIPS eligible clinician/group will not be scored on cost and the performance categories would be re-weighted as follows: Quality performance category will be re-weighted to 55% of the MIPS Final Score, the Improvement Activities (IA) performance category will be 15% and the Promoting Interoperability (PI) performance category will be 30%.
- In all performance years, the Cost performance category is assigned a weight of 0% for MIPS eligible clinicians scored under the APM scoring standard as MIPS APM participants being assessed on cost and utilization via the requirements for participation in the MIPS APM.
What determines my final MIPS Score (CPS)?
MIPS COMPOSITE PERFORMANCE SCORE (CPS) - Max Score = 100 points
Final MIPS Score = Quality Weighted Score (30%) + PI Weighted Score (25%) + IA Weighted Score (15%) + Cost Weighted Score (30%) + Complex Patient Bonus (if applicable) + Small Practice Bonus (if applicable)
- The MIPS score earned by a clinician or group for the performance period determines the adjustment applied to every Medicare Part B payment to the clinician.
- The payment adjustment occurs in the second calendar year after the performance year.
Quality Scoring (30% of score or up to 30 points toward MIPS score):
- Data Completeness Requirements: Minimum 75% data completeness is required to achieve the maximum points for each measure. You must report at least 70% of your total patients who meet the measure's denominator criteria, regardless of payer (Medicare and Non-Medicare). Less than 75% completeness will not yield any points for large practices (Small Practices will still achieve 3 points).
- Case Minimum of 20: For all Quality measures, you must report at least 20 cases, i.e., the denominator must be 20 or more for the measure to be compared against national benchmarks to earn more than 3 points. For example, a Numerator/Denominator of 19/19 will achieve only 3 points (or 0 points for larger practices), but Numerator/Denominator of 19/20 could achieve 10 points.
- No Benchmarks: Measures that are not benchmarked will (initially) receive 0 points regardless of performance (small practices will still receive 3 points). It is possible that when CMS does the final analysis of the reported data, benchmarks for these measures will have been published. The baseline period for deriving benchmarks is generally two years prior to the performance year.
- New Measures will receive a minimum of 7 points the first year and 5 points the second year - large and small practices.
- 2024 MIPS Quality Benchmarks - provides points based on performance rate. Measures that are "capped" at 7 points (even with 100% performance rates are highlighted in blue).
How Quality Score is Calculated:
Note: You cannot earn more than 100% of the maximum points for a performance category.
- Determine the maximum points you can achieve (for most providers it will be at least 60 points):
- If you are reporting a Specialty Measure Set that has less than 6 measures, the denominator for the Quality category will be re-adjusted (# of measures x 10) and your score calculated accordingly.
- If the All-Cause Hospital Readmission Measure is applicable to your group (16 or more providers), your max points will increase by 10 points (to 70). CMS will calculate your performance in this measure from Administrative Claims data. It will be scored only if your group meets the minimum case requirement of 200 for this measure, and will be added to your Quality score by CMS to determine the final MIPS score.
- For all other providers, you score will be based on 60 (6 measures x 10).
- Sample calculation #1: Based on 60 points max in the denominator: 48 (number of achievement points earned over 6 measures reported)/60 x 40% x 100 = 32 points for Quality category
- Sample calculation #2: Based on 40 points max in the denominator (if you report a specialty measures set with 4 measures: 32 (number of achievement points earned over 4 measures reported)/40 x 40% x 100 = 32 points earned for the quality category.
- Calculate Achievement Points:
- Eligible clinicians can earn maximum of 10 points* for each of the measures reported.
- The submission method, (Registry, EHR, etc.) and the corresponding benchmark will determine the points earned for each measure.
- Add in CAHPS for MIPS Achievement Points (if applicable):
- Groups and Virtual Groups can report CAHPs for MIPS survey as one quality measure towards the required 6 measures.
- Fulfills the requirement to report at least one high priority measure.
- The survey comprises 10 Summary Survey Measures (SSMs) where each SSM has its own benchmark.
- The CAHPS for MIPS Survey is also included in the improvement activities performance category as a high-weighted activity.
- Quality Improvement Scoring:
- This will be calculated for the eligible clinicians and groups that show improvement from the previous year.
- The improvement score will be calculated at the performance category level, so ECs can select different Quality measures each year.
- Up to 10 percentage points could be earned for showing an improved performance in the Quality category.
- The improvement score will be calculated as long as there is a previous year performance to be compared.
- 30% of maximum possible performance category score will be considered as the minimum baseline. Improvement will be calculated from there. So if a provider earned only 3 quality points in the current year, the quality performance improvement will be calculated on an assumed baseline of 18 points from the previous year (30% of the the maximum 60 quality points).
- Bonus points are not factored in when determining improvement score.
- Improvement Percent Score = (increase in quality performance category achievement percent score from prior performance period to current performance period / prior performance period quality performance category achievement percent score) x 10.
Promoting Interoperability Scoring- PI (can be worth 25% or up to 25 points toward MIPS total score):
- Must use 2015 Edition CURES Update (CEHRT)
- 180 days minimum reporting period (up from 90 days)
- Performance-based scoring at the individual measure level •
- CMS will require reporting of the Immunization Registry Reporting and Electronic Case Reporting (unless an exclusion can be claimed).
- The Public Health Registry Reporting, Clinical Data Registry Reporting, and Syndromic Surveillance Reporting measures will be optional and MIPS eligible clinicians could earn 5 bonus points if they report a “yes” response for any one of them. Note reporting more than one of these optional measures won’t result in more than 5 bonus points.
- A new required measure called the Safety Assurance Factors for EHR Resilience Guides (SAFER Guides) has been adopted. This measure requires MIPS eligible clinicians to attest to conducting an annual assessment of the SAFER Guides.
- Four Objectives for a possible total of 105 points weighted at 25%:
- e-Prescribing - 10 points
- Query of Prescription Drug Monitoring Program (PDMP) - 10 points
- Health Information Exchange - 30 points
- Provider to Patient Exchange - 25 points (this measure does not have exclusion criteria)
- Public Health and Clinical Data Exchange - 25 points
- e-Prescribing - 10 points
- How is Total score calculated?: To calculate your total PI score, you add up the scores from each objective + bonus points (if applicable), multiply by PI weight (25%). The following are examples of how each objective is scored:
- Example 1 e-prescribing scoring: example numerator/denominator = 50/100 = .5 x 10 = 5 points for this category. (another example: Numerator/denominator = 1/100. 1% performance rate = 1 point for this category (.1 x 10 = 1 point)). This measure is worth up to 10 points unless re-weighted. PDMP (yes) = 10 points.
- Example 2 Provider to Patient Exchange: 60/100 = .6 x 25 = 15 points for this measure. This measure is worth up to 25 points unless re-weighted higher due to exclusion of other categories.
- Example 3 HIE objectives (20 points each unless re-weighted):
- Support Electronic Referral Loops by Sending Health Information: 1200/1550 = .774 x 15 = 11.6 points (rounded up to 12 points)
- Support Electronic Referral Loops by Receiving and Incorporating Health Information: 1000/1550 = .645 x 15 = 9.7 (rounded up to 10 points)
- Example 4 Public Health and Clinical Data Exchange - 25 points for reporting to 2 different data registries - Immunization and Electronic Case reporting.
- Calculated score from examples above: (5+10+15+12+10+25) x .25 = 19.25 (out of a possible 25 PI points).
- Exclusions can be claimed for the following base measures: E-Prescribing, Health Information Exchange and Public Health and Clinical Data Exchange. If exclusions are claimed, the points for excluded measures will be reallocated to other measures:
- E-prescribing exclusion: 10 points are redistributed equally among HIE making each measure 25 (vs. 20) points. Note that the bonus measure does not have exclusions since it is optional.
- Support Electronic Referral Loops by Receiving and Incorporating Health Information exclusion: The 20 points are redistributed to the Support Electronic Referral Loops by Sending Health Information making it 40 points (vs. 20).
- Support Electronic Referral Loops by Sending Health Information exclusion: redistributes the points to Provider to Patient Exchange objective making it worth 60 points (vs. 40).
- Public Health and Clinical Data Exchange Exclusion: If you meet and claim an exclusion for one of the 2 required measures you can still receive 25 points for the objective. If you meet and and claim an exclusion for 2 measures in this objective, the 25 points would be redistributed to Provider to Patient Exchange objective making this measure worth 50 points. 5 bonus points will be awarded if you attest to 1, 2 or 3 of the optional registries.
- Note that Security and Risk analysis is required but has no point value.
- To earn a score for the Promoting Interoperability performance category, you must:
- Use CEHRT for the performance period (90-days or greater)
- Submit a “yes” to the Prevention of Information Blocking Attestation
- Submit a “yes” to the ONC Direct Review Attestation
- Submit a “yes” for the security risk analysis measure
- Conduct an annual assessment of the High Priority Practices Guide SAFER Guides (To meet this measure, MIPS eligible clinicians must attest YES)
- Report the required measures under each Objective or claim any applicable exclusions
- Each measure is scored on performance based on the submission of a numerator and denominator or a “yes or no”
- Must submit a numerator of at least 1 or a “yes” to fulfill the required measures
- The scores for each of the individual measures are added together to calculate a final score
- If exclusions are claimed, the points will be allocated to other measures
IA Scoring (can be worth 15% or up to 15 points of total MIPS score):
- You have to attest that you completed, for a minimum of 90 days, one or more Improvement Activities.
- You can earn a maximum of 40 points for this category (carries 15% weight towards the final MIPS score).
- Improvement Activities are divided into medium-weight and high-weight activities.
- High-weight activities carry twice the weight of the medium-weight activities, and therefore count twice as much towards the final MIPS score.
- Small Practices (and non-patient facing, rural, underserved) are awarded double the points for both the medium-weight and high-weight activities, thus reducing the number of activities that they need to report.
- The formula to translate the IA performance category percent score into a MIPS score contribution is:
- Sample score calculation 1 (small practice): 20 (1 medium weighted activity)/40 x .15 x 100= 7.5 points
- Sample score calculation 2 (large practice): 10 (1 medium weighted activity)/40 x .15 x 100 = 3.75 points
Cost Scoring (30% or up to 30 points towards total MIPS score):
- Per MACRA legislation, the combined weight of the Quality and Cost categories must equal 60% of the overall MIPS score. This is true in PY2021 and will remain so in future program years.
- The Cost category score will be calculated from the Medicare administrative claims. There is no additional data submission required for performance year 2021.
- The Cost performance category score for 2023 will be calculated based on 3 categories:
- Medicare Spending Per Beneficiary Clinician (MSPB)
- Total Per Capita Cost for all attributed beneficiaries
- 18 episode-based measures
- Cost is scored very much like Quality, where each measure earns up to 10 measure achievement points via benchmarks based on performance rate. Both the measures will be scored on a decile scale (0-10 points). Benchmarks are based on the performance for the same year.
- The score will be calculated when the organization meets the case minimum requirement for the two measures: 35 for MSPB and 20 for Total Per Capital Cost.
- The total available achievement points for Cost is 30.
- How is Cost performance calculated?: (Total measure achievement points) /(Total available measure achievement points)
- Sample Score Calculation: 11 (6 out of 10 measure achievement points for the Cost Per Capita measure and 5 out of 10 measure achievement points for the MSPB measure)/20 x 10% x 100 = 5.5 points for Cost Category. (11/20 x .1 x 100 = 5.5)
- Exception 1: If only one measure (i.e. only MSPB) can be scored, the score on that measure will determine the Cost Category score.
- Exception 2: If the eligible clinician or group cannot meet the case-minimum for both the Cost category measures, the weight of the Cost category (10%) will be reassigned to the Quality category (50%), making it 60%.
Bonus Scoring:
- Small Practice Bonus
- Small practices will be awarded 6 additional points in the Quality performance category score of clinicians in small practices. Organizations can find their small practice status for the 2023 performance year using the CMS MIPS Participation Tool.
- Complex Patient Bonus (10 points maximum added to final MIPS score)
- Clinicians can earn up to 10 bonus points based on the medical complexity and social risk of your patients:.
- Medical complexity as determined by the average Hierarchical Condition Categories (HCC) risk score of your Medicare patient population.
- Social risk as determined by the proportion of your Medicare patient population that’s dually eligible for both Medicare and Medicaid.
- Clinicians can earn up to 10 bonus points based on the medical complexity and social risk of your patients:.
What impact does MIPS have on my Medicare payments and clinical reputation?
- MIPS eligible clinicians will receive neutral, positive or negative payment adjustments based on their composite performance score (CPS).
- The maximum negative adjustment is 9%.
- The threshold for these payment adjustments will be the mean or median composite score for all MIPS eligible clinicians during the previous performance period. CMS estimates that approximately 572,000 eligible clinicians would be required to participate in MIPS in the 2024 MIPS performance period. Under the proposed rule, the payment adjustment for the 2026 payment year would range from - 9% to +9X% where X is an adjustment factor to allow the MIPS program to stay budget neutral.
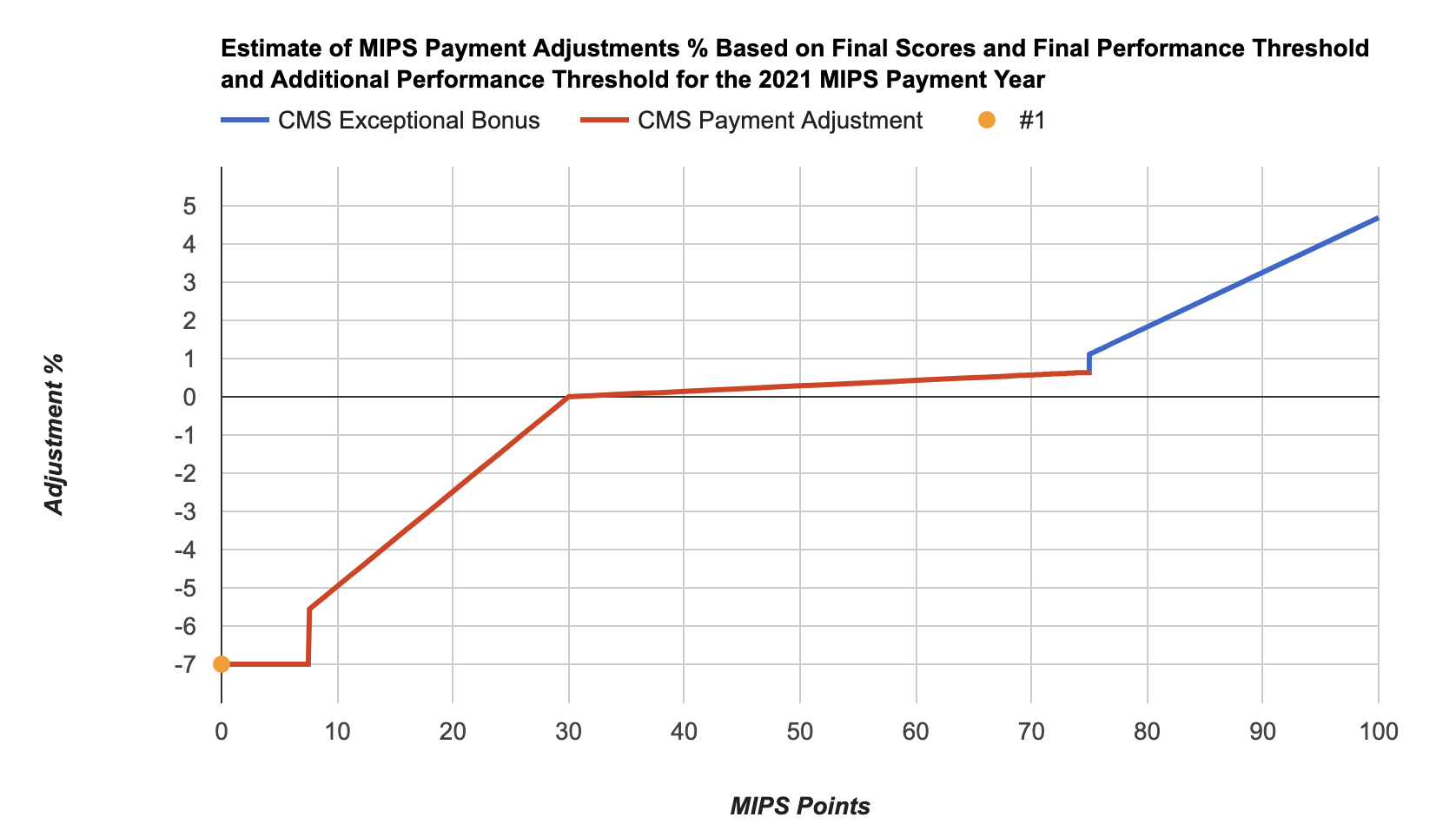
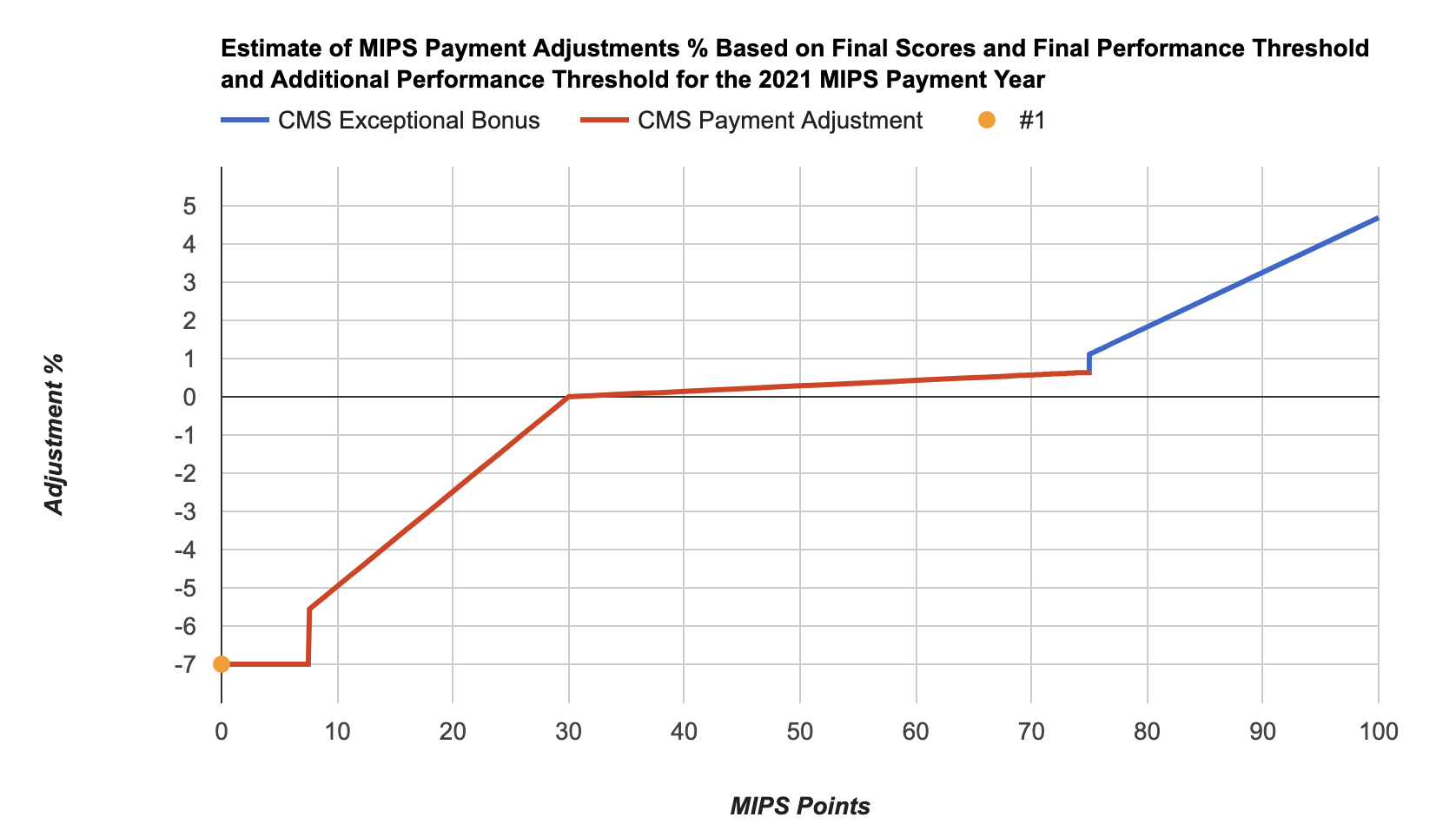
How to read this graph:
- The figure above is the CMS’ projection for how MIPS scores will translate into Medicare Part B payment adjustments for the 2024 performance year and associated 2026 payment year.
- Each year, CMS sets a performance threshold (PT) at which a provider earning at least this number of points, will receives 0% adjustment to their Medicare Part B payments – no penalty, no incentive. CMS has set the performance threshold to 75 points.
- Every incremental tenth-of-a-point corresponds to a proportional change in payment adjustment. The maximum penalty of -9% is assessed if a clinician scores below ¼ of PT (equal to 11.25 points for 2021).
- The maximum bonus is estimated by CMS to be 4.69% for clinicians that reach a MIPS score of 100 on 2024 MIPS reporting (~$6,100 for a clinician with an average $130,000 of Medicare income).
Payments excluded from MIPS payment adjustments:
- Medicare Part A
- Medicare Advantage Part C
- Medicare Part D
- CAH Method I facility payments
- Federally qualified health center (FQHC), rural health clinic (RHC), ambulatory surgical center (ASC), home health agency (HHA), hospice, or hospital outpatient department (HOPD) facility payments billed under the facility’s all-inclusive payment methodology or prospective payment system methodology
Your MIPS score moves with you!
- The financial and reputational impacts of the MIPS score are attached to a clinician, even if the clinician changes organizations/practices.
- In addition, every historical MIPS score earned by a clinician is a permanent part of the publicly-reported record released and maintained by CMS, effectively making MIPS scores an increasingly significant portion of a clinician’s resume.
Reputational Impacts:
- CMS publishes performance measures through its Physician Compare website. MACRA requires CMS to publish each eligible clinician’s annual MIPS score and performance category scores within approximately 12 months after the end of the performance year.
- The following MIPS data are available for public reporting for clinicians and groups: –
- Quality
- Promoting Interoperability
- Improvement Activities
- Cost
- Performance category scores
- Final Score
- Consumers will be able to see their clinicians rated against national peers on a scale of 0 to 100.
- A subset of MIPS quality measures will be reported as measure level star ratings.
- Measures reported as star ratings must meet the established public reporting standards. Star ratings and star rating cut-offs must prove to be reliable.
What is the minimum MIPS score I have to achieve to avoid a penalty?
Tthe performance threshold is set at 75 points.
- Objective: e-prescribing
Is there flexibility within MIPS for Small Practices?
If reporting as individuals or as a group, and your TIN has 15 or less eligible clinicians (CMS Small Practice Definition: 1-15 eligible clinicians), you might be able to take advantage of flexibility available for small practices:
- Small Practice Bonus Points:
- Small practices will be awarded 6 additional points including it in the Quality performance category score of clinicians in small practices instead of as a standalone bonus.
- You can find your small practice status on the MIPS Participation Status Tool.
- Hardship Exception for PI:
- Small Practices will automatically receive the hardship exception if they encounter overwhelming circumstances and are unable to utilize a certified EHR to fulfill PI category reporting requirements.
- Quality = 40% and IA 30% when PI re-weighted. If Cost cannot be calculated and PI is re-weighted, Quality = 50% and IA = 50%.
- Data Completeness Requirement (for Quality measures) Not Met
- A Small Practice will earn 3 points for a measure that fails data completeness of 75%% (or has less than 20 in the denominator). Practices with 16 or more eligible clinicians (large practice designation) will not earn any points for measures that are not complete.
- Double Weight for Improvement Activities
- Small Practices are awarded double the points for both the medium-weight and high-weight activities which reduces the number they need to report to achieve the full value of this category.
How do I get started reporting MIPS through MDinteractive?
You can report 3 categories of MIPS through MDinteractive:
- Quality
- Improvement Activities
- Promoting Interoperability (requires use of a 2015 Edition Cures Update CEHRT)
This is a summary of the necessary steps:
- Determine your eligibility
- Create an account - for no upfront cost - with MDinteractive (if you don’t already have one)
- Decide if you will be reporting as a group or as individuals
- Decide which categories of MIPS you will be reporting/attesting to:
- Quality
- Pick your Quality measures at MIPS by Specialty or Quality Measures
- Determine how you will collect (and then report) your data:
- Manual entry using available user-friendly software tools
- Use of excel templates to collect and report data (and then upload to secure file storage area of account
- Upload EHR files
- Check with MDinteractive to see if your existing files might be able to be used for reporting Quality data.
- Promoting Interoperability (PI)
- Run report for a minimum of 180 day date range from your Certified EHR to get data (numerator/denominator numbers) for at least the base measures.
- Enter numbers into the PI module of the software for attestation.
- Improvement Activities (IA)
- Review list of available Improvement Activities
- Choose 40 points worth of activities based on your group size (performed for a minimum of 90 days). If reporting MIPS as a group, at least 50% of the providers in the TIN must have completed the activity.
- Log into your account and from the IA module (add/edit), enter at least 90 day date range, find your activities and attest “yes”.
- Quality
- Small Practice Bonus Points:
What are MIPS Value Pathways (MVPs)?
2023, 2024, and 2025 performance years - Individual clinicians, single specialty groups, multi-specialty groups, subgroups, and APM Entities can report MVPs.
- 2026 performance year and for future years - Individual clinicians, single specialty groups, subgroups, and APM Entities can report MVPs. Multispecialty groups will be required to form subgroups to report MVPs.
CMS continues to focus on the development of MVPs and subgroup reporting and has finalized a total of 16 MVPs for the 2024 performance year.